The gastric sleeve, or sleeve gastrectomy, is the new kid on the block so to speak. It’s not a new operation. We used to do the surgeries for other reasons not including weight loss. About 15 years ago a hormone was discovered called ghrelin. It’s a hormone made by part of the stomach that makes you feel hungry. We thought if we took that part of the stomach out, we’ve actually done two things. First we’ve made you a smaller stomach so you can’t eat very much. Secondly, when you take that part of the stomach out, ghrelin levels go way down. Since ghrelin makes you feel hungry, hunger levels go way down in its absence. If you think about it, one of the potential downfalls of every single weight loss plan in the world is hunger. If we can control hunger it’s a lot easier to lose weight and keep the weight off. Sleeve gastrectomy is the fastest growing option out there. It is the most common operation for weight loss right now. Last year about 2/3 of all operations done for weight loss were sleeve gastrectomy in the US. It’s close to 95% of what I do these days because it works so well and we see a quick recovery with very low risk. It keeps your anatomy normal.
In the sleeve gastrectomy, we remove the greater curve of the stomach (stretchy part). If you eat a large meal the stomach fills and stretches way out as you eat. That’s how it can hold so much. When we remove the stretchy part it leaves you with a tubular part (or sleeve). Sometimes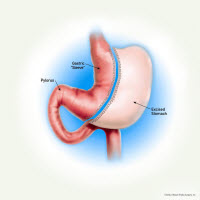 when people hear the term sleeve gastrectomy they mistakenly think we’re placing something around the stomach. We’re not placing anything around the stomach. It’s referred to as a sleeve gastrectomy because we’re changing the shape. Like the sleeve on a shirt, it’s tubular shaped. We’re making it into a tubular shape. Nothing is bypassed so there is no malabsorption. Your anatomy remains normal. Food is going to enter the stomach and empty into the small intestine the same way it did before. The size of the stomach is about the size and shape of a medium banana. The part of the stomach that’s removed is the part that makes the hormone ghrelin. Ghrelin is decreased so hunger decreases. This doesn’t mean that you won’t get hungry. There are still good reasons to get hungry. Your hunger is just much easier to control. This surgery is increasingly popular and the fastest growing option out there. It’s literally close to 95% of what I do nowadays.
when people hear the term sleeve gastrectomy they mistakenly think we’re placing something around the stomach. We’re not placing anything around the stomach. It’s referred to as a sleeve gastrectomy because we’re changing the shape. Like the sleeve on a shirt, it’s tubular shaped. We’re making it into a tubular shape. Nothing is bypassed so there is no malabsorption. Your anatomy remains normal. Food is going to enter the stomach and empty into the small intestine the same way it did before. The size of the stomach is about the size and shape of a medium banana. The part of the stomach that’s removed is the part that makes the hormone ghrelin. Ghrelin is decreased so hunger decreases. This doesn’t mean that you won’t get hungry. There are still good reasons to get hungry. Your hunger is just much easier to control. This surgery is increasingly popular and the fastest growing option out there. It’s literally close to 95% of what I do nowadays.
The surgery doesn’t take that long. It generally lasts about 45 minutes. 95% of the surgeries we do are outpatient. It’s pretty rare that someone needs to spend the night. Full recovery isn’t as fast as the adjustable bands but it’s a lot faster than gastric bypass. Most people are comfortable driving about 3-4 days after surgery. Generally in 2 weeks people can do most things. In a month you can do anything you want. Recovery tends to be really quick.
What are the risks? The first 30 days is the same as the other surgeries. It’s just slightly different numbers. In theory the death rate and leak rate should be the same as gastric bypass. But we’re not seeing that. What we’re seeing is about 1:1000 for deaths and less than half a percent for leaks. Wound infections, DVT’s, PE’s and dehydration have fewer risks than gastric bypass because the surgery doesn’t last as long. But it’s not impossible for any of those things. One of the things I really like about this operation is that we’ve gotten rid a lot of the long term risks. You’ve got normal anatomy so once you’re healed, you’re healed. The thing we have to keep in mind is stenosis. Stenosis means narrowing. Anywhere along the tubular stomach could get scarring and become too narrow. If that happened you would go see a gastroenterologist. They can look in there and take care of it. It would be very rare to need another surgery after the sleeve. In theory stenosis should be about 1%. I’ve done over 1600 of these surgeries. I’ve only seen 1 case of stenosis.
We basically see the same weight loss as we did with the gastric bypass. Average weight loss is 70% of what you were overweight. If you are 100 pounds overweight, your average weight loss will be 70 pounds. If you are 200 pounds overweight, your average weight loss will be 140 pounds. That’s average. Some will lose more and some will lose less. That is very good weight loss. Long-term we see about 10-20% regain most of their weight. With any of these operations you can gain your weight back. Your stomach is a little bigger than with the gastric bypass. So why do we see a similar result? It’s because ghrelin levels go down. In the other operations, that part of the stomach is still there. We can control the hunger somewhat with appetite suppressants. But they’re not necessarily ideal. With the sleeve gastrectomy ghrelin levels go down and hunger is easier to control.
Overall, for most people considering weight loss surgery, the sleeve gastrectomy is the better option. One of the reasons is we keep the anatomy normal. There’s a lower risk with the procedure, a fairly quick recovery and very good weight loss. We also get rid of any concerns about having anatomic abnormalities or nutritional abnormalities (malabsorption). There’s no mechanical device. Finally, you haven’t burned a bridge. That means if you don’t get out of it what you wanted out of it your anatomy is at least still normal. If your anatomy is still normal you could still have any of the other surgeries done. You could have a band placed on it or converted to a bypass. This is much more difficult after any other the other weight loss surgeries. We haven’t revised these things. We’ve seen really good results with them.
 How does CFWLS compare to the national average? Obviously we’re doing this for weight loss to improve medical problems and improve your life. We’re doing the same thing as everyone else in the world but we’re seeing better weight loss. We have a 15.8% better average weight loss at 2 years. We have good education and weight loss. We give you a full year afterward. And with that better weight loss we also see better reduction in medical problems: Diabetes 78.6% vs 62.3%, HTN 62.5% vs 46.9%, lipids 70.7% vs 45.3%, sleep apnea 69.4% vs 56.6%, and GERD 74.3% vs 16.6%. Some people think weight loss surgery shouldn’t be done on patients with GERD. But we’ve seen it get much better, not worse. Again, it’s not the operation. It’s what you do with the operation. If you do the right things it can fix these medical problems.
How does CFWLS compare to the national average? Obviously we’re doing this for weight loss to improve medical problems and improve your life. We’re doing the same thing as everyone else in the world but we’re seeing better weight loss. We have a 15.8% better average weight loss at 2 years. We have good education and weight loss. We give you a full year afterward. And with that better weight loss we also see better reduction in medical problems: Diabetes 78.6% vs 62.3%, HTN 62.5% vs 46.9%, lipids 70.7% vs 45.3%, sleep apnea 69.4% vs 56.6%, and GERD 74.3% vs 16.6%. Some people think weight loss surgery shouldn’t be done on patients with GERD. But we’ve seen it get much better, not worse. Again, it’s not the operation. It’s what you do with the operation. If you do the right things it can fix these medical problems.
 Why is the education and support so important? We have Weight Management University for Weight Loss Surgery™. It’s a 12-month post-op program. It includes all kinds of thing including the following: pre-op and post-op text books, monthly support group, 12 Weight Management University courses, access to Members Only portal, fitness classes, personal training and more.
Why is the education and support so important? We have Weight Management University for Weight Loss Surgery™. It’s a 12-month post-op program. It includes all kinds of thing including the following: pre-op and post-op text books, monthly support group, 12 Weight Management University courses, access to Members Only portal, fitness classes, personal training and more.
View the online surgical webinar and then schedule a call with Cat Williamson to go over any further questions you may have. You’ll get a copy of my best-selling book, Less Weight…More Life!






 Cat Keller has a wealth of experience in marketing, e-marketing, advertising and customer service and manages our Weight Loss Nutritional Store. She is always planning something fun and exciting. special events, discounts, giveaways – it’s never a dull moment. She is happy to help you with questions you may have regarding our products or services. Cat is a graduate of William & Mary, where she studied Government/Pre-Law and minored in Marketing.
Cat Keller has a wealth of experience in marketing, e-marketing, advertising and customer service and manages our Weight Loss Nutritional Store. She is always planning something fun and exciting. special events, discounts, giveaways – it’s never a dull moment. She is happy to help you with questions you may have regarding our products or services. Cat is a graduate of William & Mary, where she studied Government/Pre-Law and minored in Marketing.